April 4th marked the second anniversary of my open-heart surgery, and that’s given me pause to reflect on how things have gone since then. Generally, the ticker has given me no problems on its own. My blood pressure is great (taking 50mg of Losatan per day, down from 100mg). 
There is just a bit of leftover tenderness in the sternum when I perform an activity which utilizes that area. I’ve learned from my excellent trainer, Patrick Severson, how to keep things closer to the core when working out and when doing any activity. Thanks, Pat, it’s really been a help!
The main negative thing has been the blood thinner, the Coumadin – or generically, Warfarin – which I have been told I have to be on with an artificial aortic valve. It has created several different challenges for me to overcome, and I’m still learning how to deal with them. And it’s still humorous to me that I have to hold back my intake of foods rich in vitamin K – foods which everyone is told are so good for you – because they thicken the blood and counteract the blood thinner’s effectiveness. So no more Kale chips or big mounds of broccoli – or cranberry sauce, for that matter. But I’m still trying to be patient in getting in-synch with this new curve ball.
But everyday life is pretty much the same or better than it was before the surgery. Of course, I imagine that quitting the cigarettes and caffeine (and watching the salt and fats intake) hasn’t hurt in that area. I’m still doing my job, which physically gets heavy sometimes, and singing with the chorus (quitting smoking has really helped there – I can get a much deeper breath than before, and hold a phrase longer). I really feel good about being able to do all the things that I love, and I’m very grateful for it.
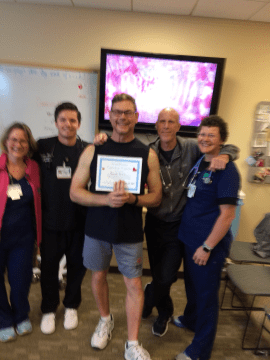
Speaking of grateful, I want to express my gratitude to the cardiac rehab team at Griffin Hospital for getting me back in shape to do these things – especially getting me ready to go back to work. They really run an excellent program there, and I’m glad I went with them instead of another hospital. So thank you to Maria, Ricky, Tom, and Trish for all the inspiration and patience you showed me. And sorry the picture of my “graduation” from the program is so out-of-focus! But it just points out how well-focused you guys are at your jobs. ❤️
And of course, my biggest thank you is to my partner Larry, without whom much of my recovery would have been so much more difficult. For all the anxiety I know my problems have caused you, and for all the good humor and patience you’ve shown in dealing with them, when you’ve already got quite enough on your plate – words cannot tell how much it’s all been appreciated.
Thanks for taking the time to read this – hopefully my story will offer help or hope to others who have to go through something like this, or to their loved ones. I hope it does. Life is good – enjoy every minute of it!





 cardboard. And it doesn’t help that I’m not using salt.
cardboard. And it doesn’t help that I’m not using salt.



 just got a call from the hospital – my surgery has been postponed until Tuesday, 4/4. My surgeon’s daughter had a baby. I guess surgeons have lives, too! Thanks to all for all the well-wishes on Facebook. They truly touched my heart (pun intended!) – and I’ll take them with me, no matter when!
just got a call from the hospital – my surgery has been postponed until Tuesday, 4/4. My surgeon’s daughter had a baby. I guess surgeons have lives, too! Thanks to all for all the well-wishes on Facebook. They truly touched my heart (pun intended!) – and I’ll take them with me, no matter when! #TBT – 18 years ago I had open-heart surgery. Everything’s been great, until just recently. I have to go in next Monday (4/3) for more work on the ticker, at Yale. I actually feel OK at this point. I’ll be having my aortic and pulmonic valves replaced (for the second time), plus a goodly part of my aorta. The problem with the aorta is called an aneurism, and I’ve got a great surgeon whose specialty is aortic aneurisms, so I should be in very good shape.
#TBT – 18 years ago I had open-heart surgery. Everything’s been great, until just recently. I have to go in next Monday (4/3) for more work on the ticker, at Yale. I actually feel OK at this point. I’ll be having my aortic and pulmonic valves replaced (for the second time), plus a goodly part of my aorta. The problem with the aorta is called an aneurism, and I’ve got a great surgeon whose specialty is aortic aneurisms, so I should be in very good shape.